Artificial Intelligence Recreates the Motion of a Beating Heart Using Surface Electrical Recordings
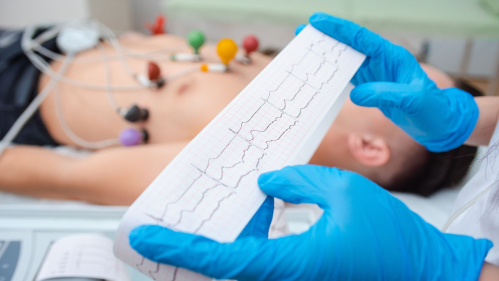
Researchers from Rutgers Health and RWJBarnabas Health have developed an artificial intelligence (AI) technology that transforms basic electrocardiogram (ECG) readings of electrical activity into sophisticated heart motion signals normally obtained via echocardiogram, potentially improving how heart disease is detected and monitored.
“ECG is very inexpensive,” said senior study author Partho Sengupta, Henry Rutgers professor and chief of cardiology at Rutgers Robert Wood Johnson Medical School and the chief of cardiology at Robert Wood Johnson University Hospital, an RWJBarnabas Health facility. “It's even present in the Apple Watch, so millions use it constantly. An echocardiogram is about 5 to 10 times more expensive than an ECG because it requires an expert moving an ultrasound device over the patient’s chest for a significant period.”
The patent-pending technology uses generative AI to assess the speed of cardiac tissue during a heartbeat using electrical signals from ECG. Then, it converts the signals to develop a speed waveform that looks exactly like the waves conventionally measured with Doppler ultrasound imaging during echocardiography. These types of signals enable doctors to see how well the heart is pumping and relaxing during a heartbeat.
This innovation addresses a critical healthcare gap: finding a way to detect heart dysfunction early with cheap and widely available tools like ECG and referring the right patients to specialists for more expensive imaging tests.
The researchers used generative adversarial networks (GANs) to train AI models that generate synthetic heart motion waveforms from electrical signals. In rigorous testing at multiple clinical sites in the United States and Canada, the technology demonstrated high accuracy in detecting both diastolic dysfunction (problems with the heart relaxing) and systolic dysfunction (problems with the heart contracting).
This approach can detect heart problems earlier than conventional methods.
“When risk factors like high blood pressure, diabetes or coronary artery disease start affecting the heart muscle, conventional measurements in ECG-detectable changes come very late,” Sengupta said. “The synthetic TDI can detect subtle longitudinal changes in heart function long before the pumping fraction decreases. The novelty is not just relying on a change in pumping fraction – also referred to as ejection fraction – but more subtle changes in heart tissue motion.”
After developing the system, the research team took several steps to validate the heart-motion waveforms it made from ECG data. When board-certified echocardiographers tried, they could not distinguish between real and AI-generated waveforms in a randomized test. The synthetic measurements also produced waveforms that varied with patient physiology and clinical parameters, such as age and blood pressure, just as real measurements do.
Most importantly, the synthetic TDI predicted outcomes.
“We found a large subset of patients in South America, with patient ECGs and follow-up until death,” Sengupta said. “Our AI was able to use their ECG data to predict death in the survival analysis long before standard ECG analysis indicated problems.”
In addition to catching more heart disease early, the innovation could prevent needless medical tests. Analysis showed the synthetic TDI technique could reduce the number of echocardiograms by 64.3% for detecting left ventricular systolic dysfunction and 69.9% for diastolic dysfunction while missing 1.4% and 6.5% of cases, respectively.
The clinical applications extend beyond screening. The technology could improve the monitoring of cancer patients receiving cardiotoxic therapies or patients with hypertrophic cardiomyopathy taking new medications that alter muscle function.
“Why do we wait for symptoms to develop when the disease starts far earlier?” Sengupta asked. “Can we find it early with screening? Can we make something equivalent to a colonoscopy for heart disease?”
The technology comes from a multidisciplinary team funded through the National Science Foundation's Bridges to Digital Health program, which brings together physicians and engineers.
“We developed everything from scratch rather than using commercial AIs,” Sengupta said.
Beyond current applications, Sengupta envisions a future with digital “twins” of patients' hearts where treatments could be tested virtually. Doctors would test treatment effects on the digital twin before choosing what to do for the real patient.
“It's almost like when you're landing on Mars, NASA creates simulations to see what works and what doesn’t before deciding to do it in physical reality,” Sengupta said. “That's how we are moving in cardiology. We want a project plan, a blueprint showing which therapy will most likely work.”
Explore more of the ways Rutgers research is shaping the future.


